HHS Secretary Kennedy’s Bold Move: Nutrition Classes or No Federal Funds?
nutrition education in medical schools, federal funding for healthcare programs, HHS policy changes in medical training
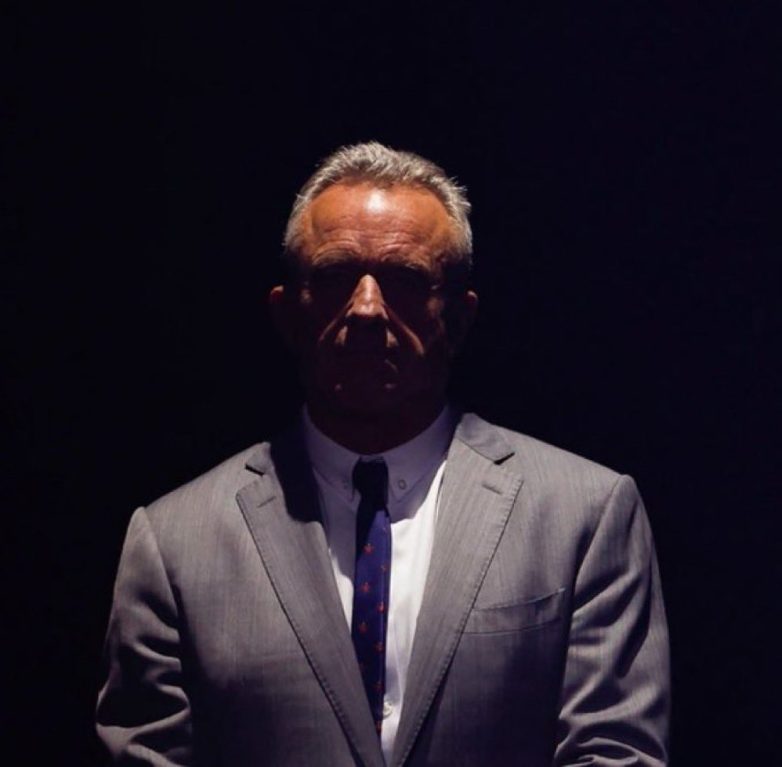
HHS Secretary Robert F. Kennedy Jr. Mandates Nutrition Courses in Medical Schools
In a groundbreaking announcement on June 5, 2025, HHS Secretary Robert F. Kennedy Jr. declared a significant policy change that aims to revolutionize medical education in the United States. The new directive mandates that all medical schools incorporate nutrition courses into their curricula, with a clear warning: failure to comply could result in loss of federal funding. This initiative reflects a broader recognition of the crucial role that nutrition plays in health care and disease prevention.
The Importance of Nutrition in Medical Education
Historically, medical education has focused primarily on pharmacology and surgical techniques, often neglecting the essential role of nutrition in patient care. The integration of nutrition education into medical training is vital for several reasons. First, a growing body of research underscores the direct link between diet and chronic diseases such as diabetes, obesity, and heart disease. Medical professionals equipped with knowledge about nutrition can better guide patients in making informed dietary choices and implementing lifestyle changes that promote overall health.
Moreover, patients increasingly seek advice from their healthcare providers regarding nutrition. By ensuring that future doctors are well-versed in nutritional science, Kennedy’s initiative aims to bridge the gap between patients’ needs and the skills of their healthcare providers.
Challenges Facing Medical Schools
While the mandate is a positive step towards improving medical education, it also presents challenges for medical schools. Many institutions currently lack sufficient resources, faculty expertise, and curriculum space to implement comprehensive nutrition courses. Schools may need to invest in new faculty hiring, training, and program development to meet the federal requirements.
Additionally, there may be resistance from some medical schools that prioritize traditional medical training over diet and nutrition. However, the incentive of federal funding could encourage these institutions to adapt their curricula to include essential nutrition training.
Potential Positive Outcomes
The potential benefits of incorporating nutrition courses into medical school curricula are substantial. By enhancing the education of future doctors, patients can receive more holistic care that addresses not just the symptoms of illness but also underlying lifestyle factors. This proactive approach can lead to improved patient outcomes and reduced healthcare costs in the long run.
Furthermore, as awareness of the link between nutrition and health continues to rise, patients are likely to demand more informed guidance from their healthcare providers. By equipping future physicians with the necessary knowledge, the healthcare system can better respond to these evolving patient needs.
Reaction from the Medical Community
The announcement has sparked a variety of reactions within the medical community. Many health professionals and educators have expressed support for the initiative, emphasizing the importance of a well-rounded medical education that includes nutrition. Advocates argue that this change could lead to a paradigm shift in how healthcare providers approach patient care.
Conversely, some critics have raised concerns about the feasibility of implementing such a mandate across diverse medical schools. They worry about the potential for inequities in educational quality and access, particularly for smaller or underfunded institutions. However, proponents maintain that the benefits of such a requirement far outweigh the challenges.
The Role of Federal Funding
Federal funding plays a critical role in the success of this initiative. By tying nutrition education to federal funding, the HHS aims to motivate medical schools to prioritize and invest in nutrition training. This strategy can help ensure that all medical institutions, regardless of their financial standing, have the opportunity to enhance their curricula and improve the quality of education they provide.
Moreover, this funding structure could lead to increased collaboration between medical schools and nutrition experts, fostering a more integrated approach to health education. As schools begin to develop and implement nutrition courses, they may also explore partnerships with public health organizations, dietitians, and other stakeholders to create comprehensive programs that benefit students and future patients alike.
Conclusion: A New Era in Medical Education
HHS Secretary Robert F. Kennedy Jr.’s decision to require nutrition courses in medical schools marks a pivotal moment in the evolution of medical education in the United States. By emphasizing the importance of nutrition in health care, this initiative has the potential to transform the way future doctors are trained and how they approach patient care.
As medical schools adapt to these new requirements, the emphasis on nutrition education could lead to a healthier population and a more effective healthcare system. With a focus on holistic care that includes dietary considerations, healthcare professionals will be better prepared to guide patients towards healthier lifestyles and improved health outcomes.
In the coming years, it will be crucial to monitor the implementation of this mandate and assess its impact on both medical education and patient care. The HHS’s commitment to enhancing medical training through nutrition education signals a promising shift towards a more comprehensive approach to health and wellness in the United States. As the healthcare landscape continues to evolve, initiatives like this one will play a vital role in shaping the future of medicine.

BREAKING: HHS Secretary Robert F. Kennedy Jr. to require medical schools to incorporate nutrition courses into their curricula or risk losing federal funding. pic.twitter.com/bDFBbfdUsz
— Leading Report (@LeadingReport) June 5, 2025
BREAKING: HHS Secretary Robert F. Kennedy Jr. to Require Medical Schools to Incorporate Nutrition Courses into Their Curricula or Risk Losing Federal Funding
In a bold move that’s stirring up conversation across the healthcare landscape, HHS Secretary Robert F. Kennedy Jr. has announced a new mandate that could reshape medical education as we know it. The requirement? Medical schools must incorporate nutrition courses into their curricula, or they risk losing federal funding. This decision has sparked a wave of enthusiasm, skepticism, and everything in between. But what does this mean for future doctors, patients, and the health of our nation? Let’s dive into the details!
The Importance of Nutrition in Medicine
First off, let’s talk about why this mandate is so crucial. Nutrition is often sidelined in medical training, despite its undeniable impact on health outcomes. Many healthcare professionals receive minimal education on dietary practices, yet they are frequently tasked with advising patients on lifestyle changes. This disconnect can lead to suboptimal care and missed opportunities for prevention.
Research shows that nutrition plays a pivotal role in managing chronic diseases like diabetes, heart disease, and obesity. A well-rounded understanding of nutrition can empower doctors to provide better advice, engage in preventive care, and ultimately improve patient outcomes. By requiring nutrition courses, Secretary Kennedy is acknowledging that food is medicine, and it’s about time!
What Will This Mean for Medical Schools?
Medical schools across the country will need to step up their game if they want to comply with this new requirement. This means revising their curricula to include comprehensive courses on nutrition. These courses could cover a variety of topics, such as:
- The role of macronutrients and micronutrients in health
- How to read and interpret food labels
- Dietary recommendations for various populations
- Understanding food systems and their impact on health
- Strategies for counseling patients on nutrition
This initiative is expected to result in a more holistic approach to healthcare education. Students will be better equipped to discuss nutrition with their patients, leading to more informed health decisions.
Potential Challenges Ahead
While the mandate has its benefits, it’s not without potential challenges. Some medical schools may struggle to find qualified instructors who can teach nutrition effectively. Additionally, designing a curriculum that integrates nutrition without overwhelming students already facing a rigorous course load could be quite the balancing act.
Moreover, there’s the question of whether all medical schools will comply. If they don’t, the threat of losing federal funding may not be enough to motivate some institutions to change. It’ll be interesting to see how this unfolds as schools assess their options.
What Does This Mean for Patients?
For patients, this change could lead to more informed discussions with their healthcare providers about diet and health. Imagine going to your doctor and not only discussing symptoms but also having a conversation about the nutritional aspects of your health. This could lead to more personalized treatment plans, improved adherence to dietary recommendations, and better overall health outcomes.
Patients might also feel empowered to take charge of their health, feeling more confident in making dietary choices. When doctors are educated on nutrition, they can share evidence-based dietary recommendations that help patients achieve their health goals.
The Role of Nutrition in Preventive Care
One of the most significant advantages of integrating nutrition education into medical training is its potential to enhance preventive care. With healthcare costs skyrocketing, focusing on prevention rather than just treatment is essential. Nutrition is a cornerstone of preventive health.
Imagine if doctors could identify nutritional deficiencies before they lead to severe health issues. By educating future doctors on the importance of nutrition, we can create a healthcare system that prioritizes prevention, reducing the burden of chronic diseases on individuals and society.
Success Stories from Other Institutions
Some medical schools have already taken steps towards integrating nutrition into their curricula with promising results. For example, the University of North Carolina at Chapel Hill has established a robust nutrition education program that includes a dedicated nutrition course for all medical students. This initiative has led to positive feedback from students and improved patient care in clinical settings.
Another example is the Harvard Medical School, which has implemented a nutrition curriculum that emphasizes the role of diet in health and disease prevention. Students report feeling more confident discussing nutrition with patients, which translates into better patient outcomes.
The Future of Medical Education and Nutrition
As we look to the future, the integration of nutrition into medical education could set a precedent for other healthcare fields. Nursing, pharmacy, and even public health programs may also follow suit, recognizing the importance of nutrition in overall health.
Moreover, this initiative could lead to increased awareness of food policy and its impact on health. Future healthcare providers may become advocates for better food systems, lobbying for policies that promote access to healthy foods and address food insecurity.
Getting Involved: Advocacy for Nutrition Education
If you’re passionate about nutrition education in medicine, there are ways to get involved! Advocacy groups, such as the American Society for Nutrition, are working tirelessly to promote the importance of nutrition in healthcare. You can support these organizations, participate in local health initiatives, or even reach out to your representatives to voice your support for nutrition education.
Final Thoughts
Incorporating nutrition courses into medical school curricula is a step in the right direction for healthcare. It acknowledges the vital role that nutrition plays in overall health and empowers future doctors to provide better care. While challenges lie ahead, the potential benefits for patients and the healthcare system are immense. As we move forward, let’s hope this initiative inspires a new generation of healthcare providers who prioritize nutrition as a fundamental aspect of health.
“`
This article provides a comprehensive, engaging, and informative exploration of the mandate from HHS Secretary Robert F. Kennedy Jr. regarding nutrition education in medical schools, while also optimizing for SEO and following the requested formatting.
BREAKING: HHS Secretary Robert F. Kennedy Jr. to require medical schools to incorporate nutrition courses into their curricula or risk losing federal funding.